The diameter of the pupil in a constant illumination condition is never the same. It is always oscillating with alternating constrictions and dilations of an amplitude up to 0.5mm (roughly up to 4% of iris diameter) and a frequency of 0.1-2 oscillations per second. Spontaneous pronounced oscillations of pupils are called “hippus.” Amplitude is decreased in bright illumination and is the largest in the average pupil size when the iris has maximum freedom of movement. An increase of oscillation amplitude of more than 1mm (that is, more than 8% of iris diameter) is observed in a number of vascular, inflammatory, degenerative and traumatic diseases of the nervous system. Often this is an early symptom of disseminated sclerosis. A decrease in spontaneous oscillations of pupils (“stone pupils”) is observed in severe neurogenic, mental, visceral and infectious diseases and also in terminal states (syncope, shock, sepsis, coma).
Unexpected, almost momentary dilations of the pupil, independent from external conditions, alternately in one or other eye, are called “jumping pupils.” In such cases, all the other reactions (concerning light, accommodation, convergention and the action of pharmacological agents) are still normal. This phenomenon takes place rarely, mostly in neurasthenia, epilepsy, myelitis, progressive paralyses, and Basedow’s disease.
Pupil reaction on light
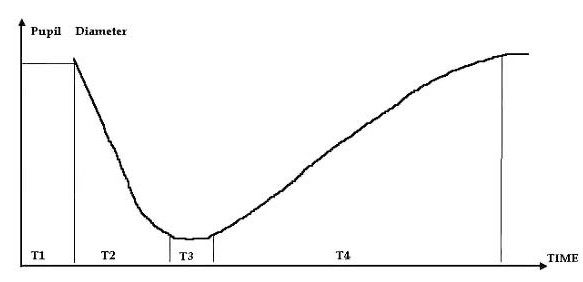
Among the various pupil reactions, the most important is the pupil reaction to light, direct and associated. Constriction of an illuminated pupil is called a direct reaction. Constriction of the pupil when illuminating the other eye is called an associated reaction. The time of pupillary reaction is known as the pupillary cycle, consisting of four parameters: latent period of pupil constriction, time of pupil constriction, latent period of pupil dilation and time of pupil dilation.
A number of violations of pupil reactions, which are the components of the classic syndromes of modern neuropathology, are described. Some of them are mentioned below.
There are three anatomical types of pupil immobility and one reflex type.
Anatomical types of pupil immobility:
1. Amaurotic immobility of pupils. In this type of immobility, both direct and associated reactions to light of both pupils do not exist, but accommodation and pupil reaction on closing an eye can still be present. Bilateral amaurotic immobility of pupils takes place as a result of the injury of both retinas or optical tract (both sides) before the primary visual centers. In such cases, double-sided blindness occurs. This is associated with considerable dilation of the pupils. If the retina or optical tract of only one eye is injured, then, in its illumination, there is no direct and associated reaction in it. When the healthy eye is illuminated, however, the direct and associated reactions are present in the blind pupil. An accommodation reaction can also still be present. It should be taken into consideration that the pupil of the blind eye is always wider. As a rule, the amaurotic immobility of a pupil develops after neuritis and atrophy of the optical nerves.
2. Hemianoptic immobility of pupils. Wernicke’s is caused by the injury of the optical tract before the lateral geniculated body. Illumination of the blind areas of the retina does not cause any direct or associated reaction of the pupil. Such reaction takes place when the intact parts of the retina are illuminated. If hemianopsy is a result of the injury, located after branching out of the pupil-motor trunk from the optical one, then hemianoptic immobility of the pupils is not present. Thereby, hemianoptic immobility of pupils occurs at the injury of the optical tract, in which the fibers of the optical nerve and light reflexes of the pupil come together.
3. Absolute immobility of pupil is characterized by the simultaneous absence of pupil reactions to light (direct and associated) and accommodation. In most cases, it is unilateral and is accompanied by mydriasis. This immobility originates in the injury of the locomotory oculomotor part of the pupil arch, starting from the nuclei of the oculomotor nerve and reaching the sphincter.
Reflex immobility of the pupils (Argylle-Robertson’s Syndrome) can be uni- or bilateral. This includes the absence of pupil reaction to light (direct and associated), more obvious than in the normal state, pupillary reaction in case of accommodation, miosis, anisocoria, smoothed relief of the iris and its partial depigmentation, sector-shaped atrophy of the iris and deformation of pupils. At the different stages of the disease, this syndrome is pronounced unequally and to different extents. First of all, pupil reaction to light is violated and its latent period is prolonged. It goes more slowly than in a normal state, and the pupils are less constricted. In some sectors of the iris, the constrictions are pronounced much strongly while in the other they are insignificant. Hyper-reflexia eventually increases and finally the reaction to light disappears completely. There are patients in which the reaction to light and other symptoms undergoes remission, but after some time, aggravation occurs. Besides the true Argylle-Roberson’s syndrome of syphilitic origin, there is the false non-specific one, observed in brain tumors, encephalitis, cranio-cerebral trauma, disseminated sclerosis, alcoholism, and so on.
Paradoxical reaction of the pupils is the dilation of the pupil at illumination and the constriction of pupils in darkness. Injury to the cortical processes of inhibition, predominantly of the paradoxical phase, is the basis of this phenomenon, which is observed in the injury of upper cervical ganglion, paralyses of the oculomotor nerve and hemorrhage to the brain ventricles.
Myotonic pupil reaction is a slowed constriction during accommodation and convergence after repeated fixing of the eyes on a remote point or a weak pupil reaction to light or its absence. Usually it is observed in one eye in disseminated sclerosis, diabetes, brain tumors and cranio-cerebral trauma.
Neurotonic pupil reaction is slowed constriction during illumination followed by slowed dilation after the light is turned off. It can be observed in vegetative neurosis, alcoholism, heavy smoking, and progressive paralysis.
Pupillotonia (Adie’s Syndrome) is a weak pupil reaction to light or its absence, a slowed accommodation reaction and slow pupil dilation up to initial size during a lengthy stay in darkness. Usually it is accompanied with anisocoria, unilateral violations as a rule and cholinegic drug sphincter hypersensitivity.
Pupil intravegetative stupor syndrome is the prolongation of the latent period of dilation. On the pupillogram, it appears like a specific plateau in the place of a parasymphatic activity transition to symphatic activity. The constriction is due to the light action and a “frozen” pupil is its iridologic sign. Apparently, the pathogenetic background is the weakening of the cholinergic component and reduction of parasympathetic tonus in chronic alcoholism.
Pupil reactions
Besides the reflex reactions to light, the following pupil reactions are also of interest:
The Cheyne-Stokes respiration pupil reactions are the absence of reactions during pauses in respiration, continuously increased dilation of pupils in forced inhalation and consequent fast return to a normal average size when decreasing the depth of breathing.
Pupil reaction on accommodation is pupil constriction when looking at objects close to the face and their dilation when looking far away. (Accommodation at a small distance is accompanied with eye convergence).
Pupil reaction on convergence is the constriction of pupils when eyes are adducted inwards, which is usually caused by a fixed look at the approach of an object. (The adduction is maximal when the object is at a 10-15cm distance from the eyes).
Pupil reaction to pain is their dilation in response to the pain or irritation. (The reflex center for transmission of these irritations to the muscle that dilates the pupil is the subthalamic ganglion, which gets impulses from the spinal-thalamic tract).
Trigeminal pupil reflex is characterized by small pupil dilation through irritation of the cornea, conjunctive eyelids or tissues surrounding the eye, which is rapidly followed by pupil constriction (present due to the connection of Y pair cranial nerves with subcortical sympathetic pupil center and additional parasympathetic ganglion of III pair nerves).
Galvanic pupil reflex is pupil constriction in response to galvanic current (the anode is placed over the eye or in the temporal area and a cathode is placed in the back part of the neck).
Cochlea-pupil reflex is bilateral pupil dilation in reaction to irritation of the vestibular apparatus (rotation etc.)
Pharyngeal pupil reflex is pupil dilation in the case of irritation of the posterior pharyngeal wall. (The reflex arc includes glosso-pharyngeal and upper laryngeal nerves.)
Pupil dilation can take place when a person is imagining night and darkness (Piltz syndrome) and constriction when imagining sunlight or a bright flame (Gaab’s syndrome); these reactions are considered to be cortical reflex reactions.